For the First Time, NYC Health + Hospitals Reaches 70% of Patients in Primary Care with Controlled Type 2 Diabetes
Poorly controlled diabetes can cause heart disease, kidney disease, and complications like blindness and amputations In the last year alone, the Collaborative Drug Therapy Management Program served over 9,000 patients and completed over 35,000 visits and the Treat to Target Program served nearly 24,000 patients and completed over 63,000 visits. After struggling to manage her type 2 diabetes for over 20 years, Chateranie Shivram improved her A1C from 11.1% to 6.7% and reduced her daily medications through the Collaborative Drug Therapy Management program
Nov 19, 2025
NYC Health + Hospitals today announced that, for the first time, 70% of its primary care patients have their type 2 diabetes controlled, a testament to the high standard of care for managing diabetes at the health system. Poorly controlled diabetes can cause blindness, kidney disease, and lower extremity amputations in adults. Most diabetes-related deaths are due to cardiovascular disease as diabetes doubles the risk of heart attack or stroke. Several programs at the health care system engage patients with diabetes, provide intensive personalized support, and connect them to additional resources as needed. In the last year, two key primary care programs, the Collaborative Drug Therapy Management Program, served over 9,000 patients and completed over 35,000 visits, and the Treat to Target Program served nearly 24,000 patients and completed over 63,000 visits. Type 2 diabetes control, measured as an A1C level below 8.0%, is a critical population health measure to track the quality of diabetes care. Today’s announcement builds on the news last month that the American Heart Association awarded twenty-three of the health care system’s primary care sites with the 2025 Target: Type 2 Diabetes Gold award, the highest possible award, for having met high thresholds for diabetes control.
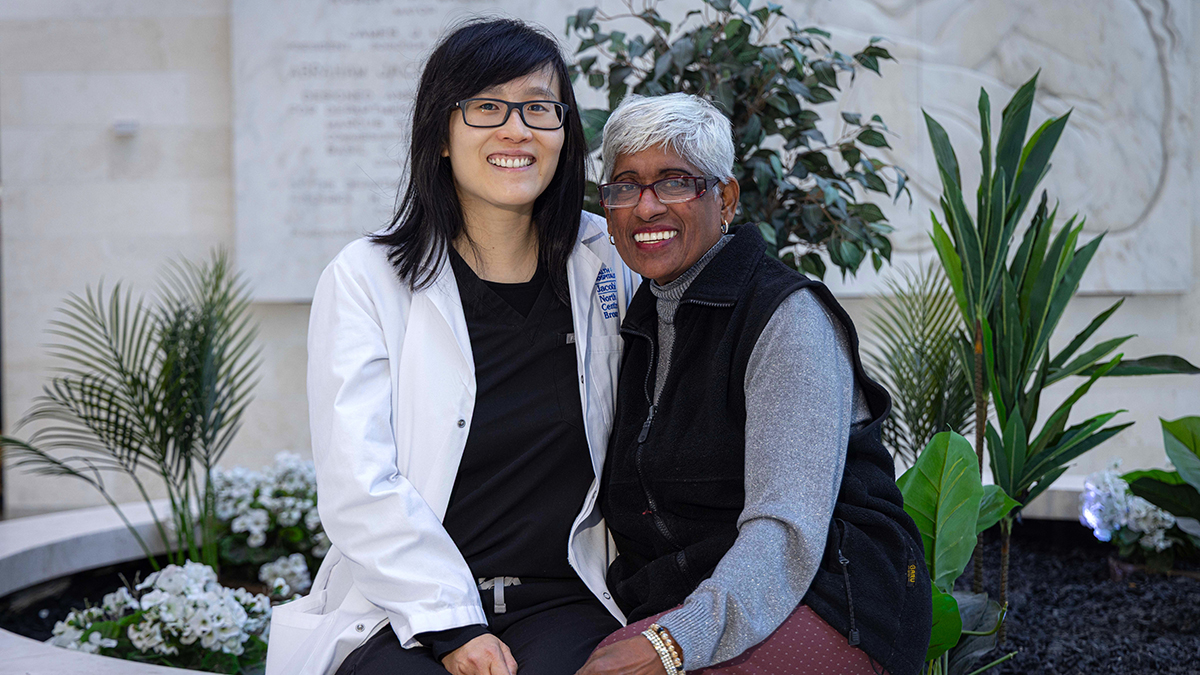
When Chateranie Shivram was referred by her doctor to the Collaborative Drug Therapy Management program at NYC Health + Hospitals/Jacobi, she had an A1C of 11.1% and had struggled to manage her type 2 diabetes for over 20 years. Over 14 months, she met monthly with pharmacist Carmen Chow to simplify her medication regimen from six medications a day to two and reduce her insulin dose by approximately 40%. As part of the program, Shivram also learned how different foods and physical activity affected her A1C level. Today, her A1C is 6.7%.

“Ms. Chow helped me a lot with my A1C level. She’s amazing,” said Chateranie Shivram, a patient in the Collaborative Drug Therapy Management program at NYC Health + Hospitals/Jacobi. “I feel much better with the medication she put me on, and I feel healthier because she removed some of my medications.”
“The most rewarding aspect of working with patients enrolled in our program is seeing their confidence grow as they gain a better understanding of their condition and start achieving measurable improvements, such as lower A1C levels, reduced insulin needs, weight loss, and fewer complications,” said Carmen Chow, PharmD, BCPS, BCIDP, Ambulatory Care Pharmacist at NYC Health + Hospitals/Jacobi. “Our Chronic Disease Management team here at Jacobi Hospital is highly collaborative and robust- patients who need additional support can also meet with our dietician or health coach for personalized guidance and extra assistance.”
When Jaime Siesquen was referred to the Treat to Target program at NYC Health + Hospitals/Gotham Health, Roosevelt, he had a lot of questions about diabetes and the medications he was prescribed. He worked with nurse Pascale Kebreau to learn about the role of insulin in the body and the importance of regular blood glucose monitoring. They also found ways to adjust his diet and exercise routine, emphasizing healthier choices like eating more vegetables, fewer refined starches, and incorporating more physical activity. Within 3 months, Siesquen achieved his A1C and weight goals and graduated from the program. His A1C dropped from 7.6% to 6.6%, and he lost 14 pounds.
“Nurse Kebreau gave me very good guidance regarding my health problems,” said Jaime Siesquen, a patient in the Treat to Target program at NYC Health + Hospitals/Gotham Health, Roosevelt. “My health has improved a lot. I have more energy to do any kind of work.”
“I help patients get better glycemic control, have fewer hospital visits, and equip the patient with the knowledge and skills to take care of themselves,” said Pascale Kebreau, RN, a nurse in the Treat to Target program at NYC Health + Hospitals/Gotham Health, Roosevelt. “It is very rewarding to me. I feel joyous and a great sense of professional satisfaction in achieving positive diabetes outcomes.”
Nearly one million New Yorkers have diabetes, and approximately 20% are undiagnosed. New Yorkers with obesity are twice as likely to have diabetes compared to adults without obesity. Adults living in high-poverty neighborhoods are also at least twice as likely to report having diabetes compared to adults living in low-poverty neighborhoods. The average medical expenditure for people with diagnosed diabetes is about $19,736 per year, with about $12,022 being attributed to diabetes directly.
“Congratulations to our care teams for attaining this incredible milestone! This is a culmination of many years of dedicated work at every level of our organization,” said NYC Health + Hospitals Senior Vice President of Ambulatory Care and Population Health, Ted Long, MD, MHS. “Managing type 2 diabetes is part of the foundation of primary care and is critical to reducing the risk of heart disease, stroke, kidney disease, and many complications. Achieving this remarkable outcome for our patients with diabetes affirms our mission to deliver the highest quality care to NYC, without exception.”
“Now, more than ever, control of chronic diseases such as diabetes is the key to unlocking better health for our patients and our communities; indeed this has long been a high priority for NYC Health + Hospitals,” said NYC Health + Hospitals Chief Medical Officer of Ambulatory Care Andrew B. Wallach, MD, FACP.
“At NYC Health + Hospitals we care for many patients with diabetes. We have developed an incredible toolkit for the front lines to be able to provide the best quality of care,” said NYC Health + Hospitals Vice President and Chief Population Health Officer Nichola Davis, MD, MS. “If you have diabetes, you’ll have a team of people on your side to help you achieve your treatment goals, including your provider and nurse as well as additional support from a clinical pharmacist, dietitian, or community health worker.”
“The Collaborative Drug Therapy Management and Treat to Target programs help bridge the gap between PCP appointments and offer patients personalized care that complements their primary care treatment,” said Lakshmi Paruchuri, MD, Primary Care Provider at NYC Health + Hospitals/Jacobi. “With the support of the pharmacists and nurses, patients have better control over their medications, blood glucose levels, and overall health outcomes.”
These results highlight the high standard of care for diabetes across primary care at NYC Health + Hospitals. Primary care providers have many tools in their toolkit to support patients with diabetes and prediabetes, including the following programs:
- Clinical Pharmacists in Primary Care – Under the Collaborative Drug Therapy Management program, clinical pharmacists are integrated members of primary care team to help patients with diabetes.
- Treat to Target – Intensive nurse-led hypertension and diabetes management primary care program for patients who are above their target.
- Chronic Disease Outreach – Nurses and outreach staff contact over 1,000 patients each month with high blood pressure or diabetes to keep them engaged in primary care, with a focus on patients who are uncontrolled and do not have an upcoming visit scheduled.
- Community Health Workers – Community Health Workers meet regularly with patients to identify and address barriers to health and well-being, such as housing, financial, food, and legal needs, as well as helping them schedule healthcare appointments and coordinate transportation.
- Teleretinal Screening in Primary Care – Primary care sites offer teleretinal screenings as part of a routine visit for patients with diabetes, instead of requiring a separate ophthalmology appointment.
- Text Messages and Support for Insulin Adjustment – This text-based program optimizes insulin dosing for patients who are on insulin.
- Text Messages and Support for Transitioning from Insulin to GLP-1 Medications – This text-based program helps patients who have well-controlled type 2 diabetes on basal insulin transition over to GLP-1 medications, which lower the risk of abnormally low blood sugar and, in many patients, lead to improved cardiovascular and metabolic health.
- In-person Educational Support in Primary Care – This includes diabetes classes, one-on-one sessions, patient support groups, and individualized dietitian support.
- Lifestyle Medicine Program – This is a several-month program to support patients in making evidence-based lifestyle changes, including a healthful plant-based diet, increased physical activity, improved sleep habits, stress management, avoidance of substance use, and stronger social connections. Adults living with prediabetes, type 2 diabetes, high blood pressure, heart disease, or health concerns related to excess weight are eligible to enroll.
- Diabetes Prevention Program – Evidence-based and structured year-long program designed to help prevent diabetes, especially among patients with prediabetes.
- Weight Management and Bariatric Surgery – Programs available to help patients sustainably achieve their long-term weight loss goals, which often leads to improved diabetes control or even resolution.
- Specialty Referral – Specialty referrals to endocrinologists, cardiologists, nephrologists, ophthalmologists, podiatrists, and many others who work closely with diabetes patients to help improve outcomes and manage or reduce their risk of diabetes-related complications.
###
MEDIA CONTACT: Press Office
#197-25
About NYC Health + Hospitals
NYC Health + Hospitals is the largest municipal health care system in the nation serving more than a million New Yorkers annually in more than 70 patient care locations across the city’s five boroughs. A robust network of outpatient, neighborhood-based primary and specialty care centers anchors care coordination with the system’s trauma centers, nursing homes, post-acute care centers, home care agency, and MetroPlusHealth —all supported by 11 essential hospitals. Its diverse workforce of more than 46,000 employees is uniquely focused on empowering New Yorkers, without exception, to live the healthiest life possible. For more information, visit www.nychealthandhospitals.org and stay connected on Facebook, Twitter, Instagram and LinkedIn.